Today we are going to introduce Mr. Ryan Begley one of our MPhys (Medical Physics) graduates. Ryan has started his PhD in neurophotonics at the school of physics, UWA.
For his PhD, Ryan is building a laser microscope and using this to image individual neurons and investigate the functional changes produced by terahertz radiation.
The title of his Masters project was: “A Small-Animal Model of Radiotherapy”, supervised by Adj/Prof Martin Ebert.
Ryan was awarded High Distinction in his Masters and his performance and research outcome was highly recognized.
Here are comments from his principal supervisor:
A novel small-animal radiotherapy device had been ordered for Perth and the manufacturer had provided the planning software ahead of the device. Ryan undertook a comprehensive study of the nature of the dose distributions the device could achieve in the small and intricate anatomy of a rat. With the kind assistance of clinical physicists from the Sir Charles Gairdner Hospital, Ryan was able to compare these distributions with those that could be achieved with human clinical devices including the CykerKnife robotic radiotherapy device. Ryan’s work established the superiority of the small-animal device, especially for radiation studies in response of the rat brain, and has been of significant help in informing research work being undertaken in pre-clinical radiotherapy research. Ryan compiled his work for presentation at the Engineering and Physical Sciences conference in Sydney in November 2016. Ryan is a highly critical and strongly independent thinker and, combined with an unwavering enthusiasm, will see Ryan achieve in whatever area he chooses to move into.
 Ryan presenting his research outcomes at EPSM conference in Sydney, November-2016.
Ryan presenting his research outcomes at EPSM conference in Sydney, November-2016.
Ryan kindly accepted to answer a few questions about his experience in our Medical Physics Research Group.
– Introduction and your current position and role:
I completed my Masters in Medical Physics at the University of Western Australia in 2016 and am now a PhD student at UWA. I am currently building a laser microscope for volumetric tissue imaging at the cellular scale and plan to use this to study the effect of terahertz radiation on the connections between brain cells in living animals.
– What did you enjoy most about UWA, and Medical Physics research group?
Having an interest in both physics and neuroscience I was naturally drawn to the Medical Physical research group as it allowed me to combine these interests in a way not offered by any other group. While there I assessed the performance of a new radiotherapy device in terms of its performance in brain cancer treatment. The support I received from my supervisor and other senior researchers in completing my project was exceptional and the coursework was enjoyable and applicable to my research project.
– Can you give us your top three reasons to study Medical Physics?
Aside from allowing me to combine my interests in physics and neuroscience, studying medical physics appealed to me as a practical means of using my knowledge to improve the health of individuals. It also gave me a great background in common applications of physics in medicine going forward into a career in research in bio-physics where medical applications are a significant driving factor.
– How do you feel you have made a difference in your field of research?
My research conducted during my Masters in Medical Physics showed that the new radiotherapy device was more precise than the latest clinical devices for brain cancer treatments in pre-clinical research. This finding allows for further research to proceed with confidence in the development of improved radiotherapy practices. The brain is particularly susceptible to the negative side-effects of inaccurate radiotherapy which includes permanent decreases in cognitive function and memory. Improved techniques have the potential to reduce these negative effects in brain tumour patients which will lead to significant improvement in their quality of life.
– What is your best advice to current students and Medical Physics applicants?
The senior members of the research group are great mentors; take advantage of their experience and generosity. Be open to new information about what medical physics has to offer and network with the people you work with during your project. Most of all make sure to pursue what you enjoy and work hard.
Once again we congratulate Ryan for his achievements and wish him all the best in his future career.
Here is the abstract of Ryan’s Masters thesis:
Background
Small-animal radiotherapy devices (SARD) allow precise irradiation for pre-clinical studies of radiotherapy. Recently developed devices mimic human treatments with low energy X-ray beams. The brain is a region where dose accuracy is particularly important due to the proximity of small, sensitive structures.
Aim
This study assesses the accuracy of a SARD and compares this with two human clinical systems; volumetric arc therapy and CyberKnife.
Method
Treatment plans were produced for two situations in the rat; irradiation of a brain tumour target and irradiation of the unilateral hippocampus. Generalised organ-at-risk (OAR) structures representative of typical clinical scenarios were outlined. The tumour target was planned with a prescribed dose of 3 Gy to 90% of the target. Past research has found that total doses of 1.8 – 2 Gy induce toxicities in the hippocampus and optic nerve. These values were used as the threshold for the small OAR. This study also compared the SARD and clinical systems in selectively targeting the unilateral hippocampus.
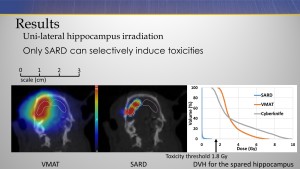
Results
CyberKnife achieved the highest dose conformity followed by the SARD and then VMAT. For targets adjacent sensitive structures such as the hippocampus or optic nerve, only the SARD platform could keep the dose below threshold.
Discussion
The SARD was theoretically the only platform successful in selectively inducing toxicities in the unilateral hippocampus. The differences in precision arise primarily from beam energy and beam delivery geometry. The steeper gradients better represent those achievable in human clinical treatments, scaled relative to the anatomy of humans and small animals, allowing for better translational research.
Here is a slide from Ryan’s presentation. It shows better dose conformality using SARD compared to a VMAT plan.
 Click on the image to enlarge.
Click on the image to enlarge.


